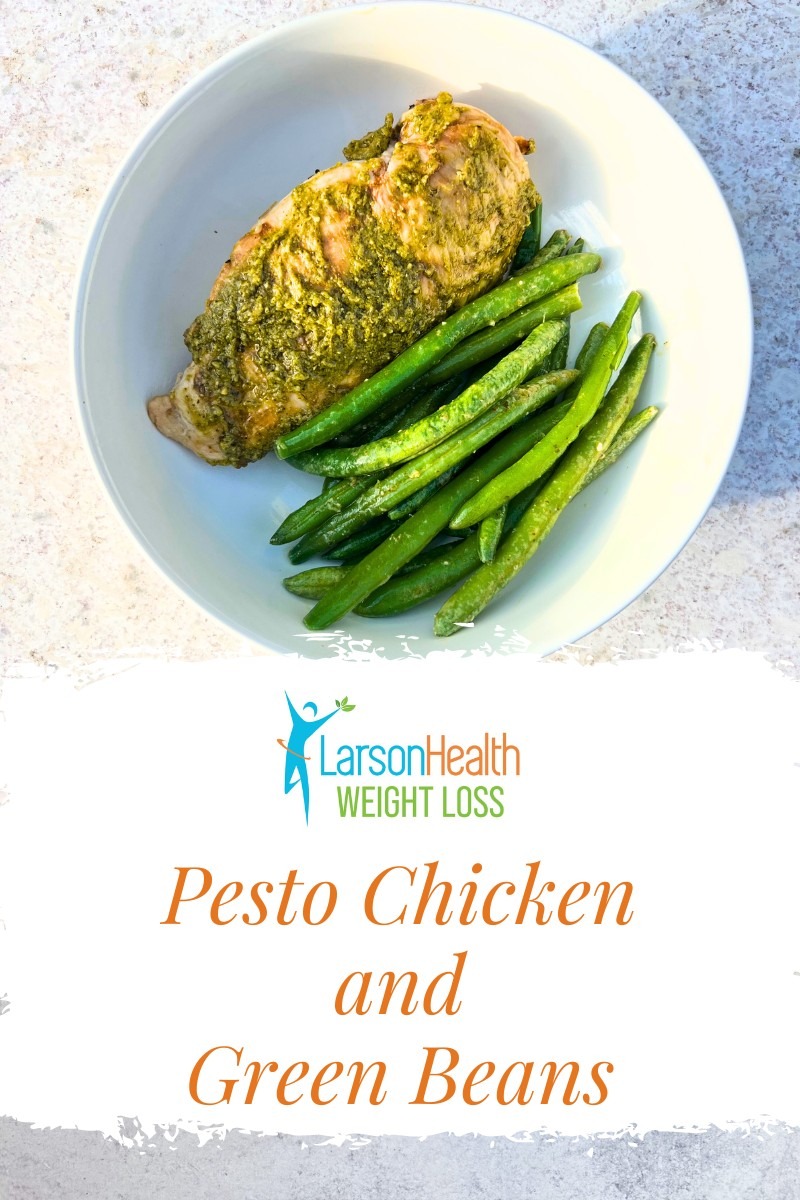
Ingredients
- 4 tbsp (50g) pre-made pesto sauce made with olive oil
- 3, 5oz (142g) boneless, skinless chicken breasts
- 8 oz (227g) green beans, trimmed
- 1 tbsp (14g) olive oil
Directions
- Warm large skillet on the stove over medium heat.
- Coat chicken breast with pesto sauce.
- Add chicken to the skillet and cook for 8 minutes on one side.
- Flip the chicken and add green beans and remaining olive oil.
- Cook until chicken is cooked through (internal temperature of 165 degrees Fahrenheit).
Nutrition Info
Calories: 305, Carbohydrate: 7, Protein: 38, Fat: 13
 Add Row
Add Row  Add
Add 










Write A Comment