Welcome to the Inner Connection Series — a multi-layered look at how our body systems communicate in ways we’re only beginning to understand. Today, we're exploring one of the most dynamic and misunderstood relationships in the human body: the gut-brain axis. What was once considered pseudoscience is now the focus of leading-edge research in neuroscience, psychiatry, immunology, and nutrition.
This isn’t just about digestion or bloating. This is about your memory, your moods, your clarity, and your overall sense of well-being.
🌿 Your Inner Ecosystem: The Foundation of Gut-Brain Health
Inside your gastrointestinal tract lives a bustling world of microbes—trillions of bacteria, viruses, fungi, and archaea. This gut microbiota outnumbers your own human cells and collectively weighs about three pounds—the same as your brain.
These microbes do more than just help digest your food. They:
Ferment fiber into short-chain fatty acids (SCFAs)
Synthesize essential vitamins
Train the immune system
Communicate directly with the brain via neural, immune, and endocrine pathways
When in balance, this ecosystem supports brain function and emotional resilience. But when disrupted—known as dysbiosis—the impact can ripple far beyond the gut.
🧾 Key Reference: Carabotti et al., 2015, "The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems." PubMed
🔄 The Gut-Brain Axis: Your Two Brains in Constant Conversation
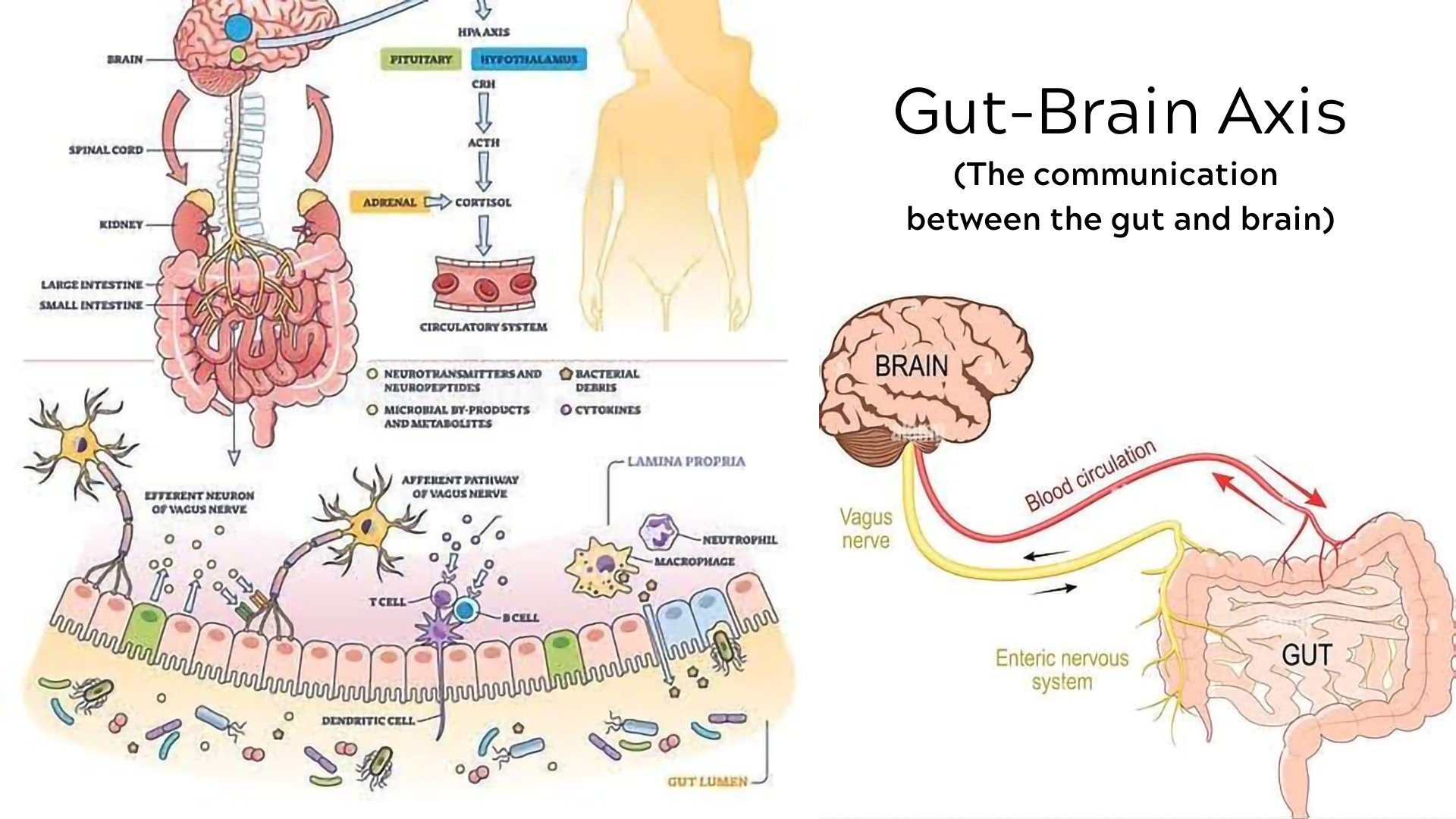
The gut-brain axis is a bidirectional communication highway linking the central nervous system (CNS) with the enteric nervous system (ENS). The vagus nerve is the main “wiring” connecting the two, but this axis also involves:
Immune signaling (cytokines)
Microbial metabolites (like SCFAs)
Hormones (like cortisol and serotonin)
What's fascinating is that over 90% of the body's serotonin—a neurotransmitter central to mood—is produced in the gut, not the brain. This is why the gut is often referred to as the “second brain.”
🧾 Key Reference: Breit et al., 2018, “Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders.” PubMed
🔍 Dysbiosis and Mental Health: What the Research Shows
Recent studies are drawing undeniable connections between gut microbial imbalances and conditions such as:
Depression
Anxiety
Brain fog and chronic fatigue
Cognitive decline, including Alzheimer’s
In one 2020 review published in Frontiers in Psychiatry, probiotic supplementation significantly reduced symptoms of depression in both healthy individuals and those with major depressive disorder. Another 2023 study in Psychiatry Research found that anxiety-prone individuals had lower levels of key anti-inflammatory gut bacteria, like Faecalibacterium and Bifidobacterium.
🧾 Key References:
Nikolova et al., 2021, “Gut microbiota in mood and psychiatric disorders." PubMed
Liu et al., 2023, “Altered gut microbiota composition in generalized anxiety disorder." PubMed
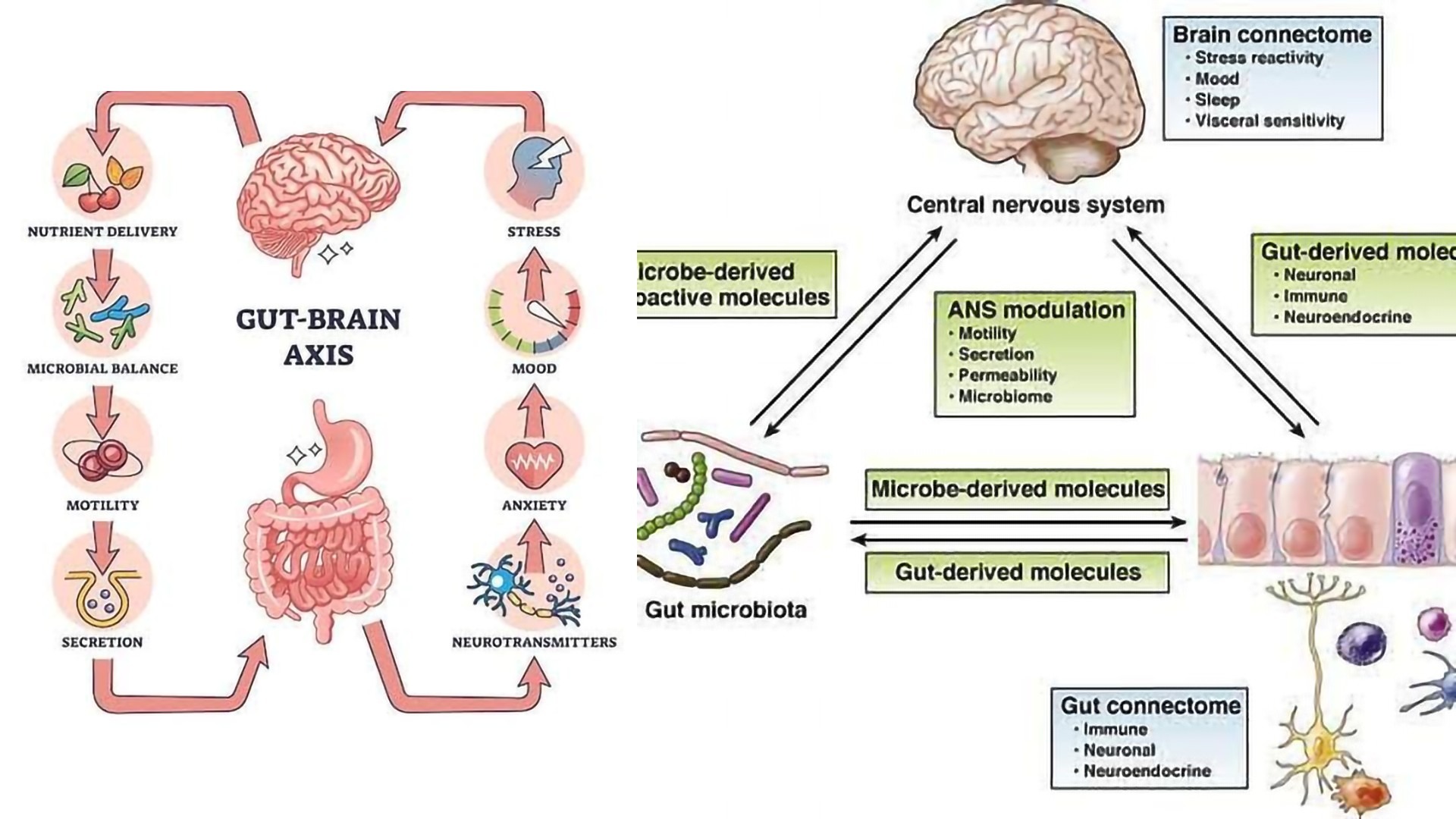
🌱 Nutritional Psychiatry: Feeding the Brain via the Gut
The science of nutritional psychiatry is emerging to bridge the gap between food and mood. Several nutrients play a role in gut-brain signaling:
1. Prebiotic fibers: fuel for your beneficial gut bacteria
Found in: garlic, leeks, oats, bananas, artichokes
Effect: Increase SCFA production → lower inflammation + support brain plasticity
2. Fermented foods: live microbes that populate your gut
Found in: yogurt, kefir, kimchi, sauerkraut
Effect: Improve microbial diversity, regulate neurotransmitters
3. Amino acids from protein: building blocks for serotonin and dopamine
Found in: eggs, fish, legumes, poultry
Effect: Tryptophan → serotonin | Tyrosine → dopamine
🧾 Key Reference: Mittal et al., 2017, “Neurotransmitters: The Critical Modulators Regulating Gut-Brain Axis." PubMed
🧬 Leaky Gut, Leaky Brain?
When the intestinal lining becomes permeable—a condition often called “leaky gut”—larger molecules like LPS (lipopolysaccharides) can cross into the bloodstream. This can trigger systemic inflammation, immune activation, and even impair the blood-brain barrier (BBB), making the brain more vulnerable to toxins and inflammatory compounds.
In one study, researchers demonstrated that germ-free mice (with no gut microbiota) had significantly more permeable BBBs, and colonization with beneficial microbes restored BBB integrity.
🧾 Key Reference: Braniste et al., 2014, “The gut microbiota influences blood-brain barrier permeability." PubMed
⚖️ Stress and the Gut: A Two-Way Street
Stress disrupts the gut microbiota, lowers digestive enzyme production, and increases gut permeability. Cortisol—the stress hormone—can thin the gut lining and inhibit the growth of beneficial bacteria.
At the same time, a disrupted gut can worsen your body’s stress response. This can create a vicious cycle: gut dysbiosis → poor stress resilience → more gut dysfunction.
Tools like meditation, breathwork, sleep, and adaptogens (ashwagandha, rhodiola) can help regulate this cycle.
🧾 Key Reference: Foster et al., 2017, “Stress & the gut-brain axis." PubMed
🧠 Smart Strategies to Support Gut-Brain Harmony
Here’s how to start healing and supporting your gut-brain axis today:
Strategy |
Why It Works |
Eat more fiber (30g+/day) |
Feeds SCFA-producing bacteria |
Add 1–2 servings of fermented foods daily |
Increases microbial diversity |
Limit ultra-processed foods |
Reduces endotoxin load |
Try intermittent fasting or time-restricted eating |
Enhances autophagy and microbial balance |
Practice stress reduction |
Calms vagal tone, improves motility |
Sleep 7–9 hours |
Gut bacteria follow circadian rhythms too |
🌟 Final Reflections: Your Gut is Talking. Are You Listening?
This isn’t about trends or gimmicks—it’s about understanding one of the most powerful, evidence-backed relationships in your body. The gut-brain axis is not only real, it’s revolutionizing the way we treat everything from IBS to anxiety to early neurodegeneration.
Start small. Choose one thing to shift this week—a daily serving of fermented veggies, a prebiotic-rich breakfast, a mindfulness practice before dinner. These tiny habits nourish an entire ecosystem, which in turn can nourish your brain.
Healing isn’t linear. But the signals your body sends you—from bloating to brain fog—are invitations to tune in, not tune out.
📚 References
Carabotti et al., 2015 – PMID: 25830558
Breit et al., 2018 – PMID: 29593576
Mittal et al., 2017 – PMID: 27870363
Braniste et al., 2014 – PMID: 25411471
Foster et al., 2017 – PMID: 28039826
Liu et al., 2023 – PMID: 36481063
Nikolova et al., 2021 – PMID: 33878834
 Add Row
Add Row  Add
Add 









Write A Comment